We meet with all kinds of opinions and recommendations, which are so frequently and with absolute certainty repeated by various experts and authorities, that they seem to be any doubtless, erstwhile and for all established truth. This applies to many areas, but medicine is an excellent example. Strangely enough, whenever I effort to take a closer look at any medical recommendations by checking and analyzing sources, these recommendations may prove unfounded, taken from the air, arbitrary, powerfully stretched or simply wrong.
Let's look at the case, it would seem the least debatable, or overweight. They say it like parrots all doctors, nutritionists, journalists and who else. Overweight is bad for your health. You want to live long and healthy, lose weight. A deafening choir. any authorities repeat even more authority. But what weight is optimal? The planet wellness Organisation (WHO) classifys BMI ranges into categories to represent different levels of wellness hazard [1, 2]. The possession of BMI in terms of underweight (BMI <18.5 kg/m2), overweight (BMI ≥25 kg/m2) or obesity (BMI ≥30 kg/m2) is considered to be a hazard origin for wellness problems and premature mortality. Only the perfect weight, or BMI in the scope of 18.5-25 is healthy. specified criteria have been adopted and are widely applied. According to them, doctors instruct patients.
It would seem that specified categorical and far-reaching statements, in addition to those decreed by the planet authority for all people around the world, should be based on the unquestionable results of many solid and serious research. The best basis could be a systematic review of all available studies by a squad of independent researchers. The review should then be continued as further studies appear and recommendations possibly updated. In the meantime, there were fewer specified studies and their analysis was not carried out. On the organisation's website you will find information mainly on the subject of anthropometric measurements and analyses and the calculated ratios for the population, while there is no mention to circumstantial work demonstrating the wellness impact of BMI. The WHO may be given the impression that the above categories of BMI were taken from the air and were made entirely arbitrary. And that is most likely the case, due to the fact that according to many opinions this is simply a typical behaviour of this institution. It makes categorical recommendations for the full planet with universal force without giving a basis for investigation results.
I think it's easy to explain. Referring to circumstantial studies would open the door to discussion. Published studies can be analysed, their limitations and weaknesses demonstrated and proposals discussed. fresh studies could lead to a change of position or call into question the sense of the recommendations, recognising the WHO as a fallacious and 1 with which it can be argued. Meanwhile, the WHO recommendations on all issue are categorical, do not let discussion, and they are mandatory and permanent. Sometimes they're changed, but it's done quietly and without explanation. simply on the website of this institution without any comment the old text disappears without trace, replaced by a fresh version. The definition of the vaccine has late been amended to include the most fresh medicinal products injected. This is more like the behaviour of spiritual sect leaders. Worse still, questioning the WHO's recommendations is very badly seen and heretics severely punished. A investigator who dares to do so may lose his sources of backing and pay for it with his professional career. This is what evidence - based medicine is now — we will prove to you that you are nothing. These are the sources of many recurrent “truths” in medicine, which frequently have no another basis, apart from the WHO recommendation, for which they repeat national medical centres. However, it is adequate for all doctors to parrot the authoritative version without exception. It is not worth the effort by studying the technological work on your own just to put yourself at risk, giving opinions or giving advice contrary to the mainstream. However, no 1 has yet succumbed to authoritative recommendations and procedures, specified as nonsense, groundless, harmful, or even deadly, they would not be.
For the above reasons, despite the importance of the subject, there is small research. These researching the relation of obesity with another diseases are mostly poorly planned and can be utilized to find at most co-occupation and correlation. For example, they do not decide whether obesity is the origin of diabetes or vice versa, or whether they simply both have common causes, which is most likely. The same applies to another diseases.
Studies demonstrating a longevity (or death hazard for all causes) relation with body weight (BMI) may be conclusive. They have the undoubted advantage of eliminating the impact of sources of mistake specified as medical diagnosis, interdependency of various diseases, etc. A simple and unambiguous assessment is adequate here, either individual is alive or not. Among the different conditions for medical examinations, specified a circumstantial examination should in peculiar comply with the following. First of all, erstwhile we survey mortality, we gotta do it for at least 10 to 15 years. Secondly, the survey group should be large enough. Third, the selection of persons for the survey group should meet the criteria for age, social, etc. in order to destruct the impact of factors another than BMI. It follows from these conditions that, despite its simplicity, specified a survey requires considerable resources and unchangeable backing for many years, which is not easy. respective specified studies have been done in the planet and it is time to discuss their results. It is worth paying attention to the dates, as the studies are later than the WHO recommendations.
The subjects were measured and weighed and then grouped by BMI size according to WHO classification. In studies with a adequate number of subjects, classification was besides performed on the basis of another factors. On the basis of mortality, the hazard of death for BMIs was determined over a given period. All hazard values were then divided by its value for the BMI group 18.5-25, which was taken as a benchmark, receiving a hazard to that group (for it by definition the comparative hazard is equal to 1). The final results of the work sometimes vary, but they all contradict authoritative recommendations, so as an example, I present a graph made on the basis of aggregate results from the latest cited work [3], which describes a survey carried out in Canada.
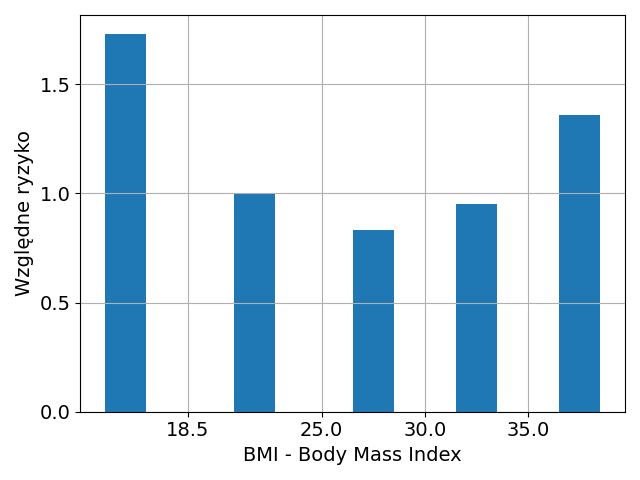
As you can see, underweight is the biggest hazard factor, even greater than obesity. From the point of view of longevity, BMI in the 25-30 scope classified by WHO as overweight, but even average obesity is not a threat. The authors of the publication effort very hard to discuss the results in a way that hides the fact that they are in clear contradiction to authoritative recommendations.
You can be tempted to have a deeper discussion. First, the chosen measure, or BMI, is imperfect. She looks very learned with that square, and so on, but she may be misleading. If the tall individual were a proportionally scaled copy of the low one, its volume, and thus the weight of the body would change according to the 3rd (cube) alternatively than the second (square) growth power. This is not the case, as the proportions of low and advanced people are mostly different. However, in more detailed tables, the recommended BMI values depend on growth, which should be borne in head by those with growth another than the average. In addition, BMI models are not suitable for children for whom another more detailed criteria are applied in the full table book. Wikipedia's English-language website on BMI quotes the opinion:
BMI tables are excellent for identifying obesity and fat in large populations, but are much little reliable for determining fat in individual individuals.
A number of alternate measures have so been proposed, but BMI is now officially utilized and any investigation should mention to it, while alternate measures can be utilized in parallel.
Body weight is dependent on many factors, especially composition. Muscles are heavier than fat, so it can happen that an athletic individual will be classified as obese. More detailed studies besides propose that, for example, the subcutaneous fat layer does not pose a wellness risk. Since abdominal obesity, in which fat is deposited on the interior organs, is considered to be peculiarly dangerous, it has been suggested that a better wellness indicator than BMI, despite its simplicity, may be a belt circuit, possibly referred to growth. specified a measurement proved more sensible, especially for children and teenagers [7], where a simple advice that the circumference in the waist should not be larger than half the height, works much better, and a part of string is adequate to measure. We, too, should pay more attention to the matching of trousers than to the indication of weight, erstwhile we are in fashion and decide to "take care of ourselves."
In any case, its composition (muscle mass) and metabolic wellness are more crucial than body weight. The English-language word "skin fat", or thin fat, describes an individual with a slim appearance with a average BMI, but having excess body fat, but not much muscle. This reasonably common condition, not only in the elderly, has nothing to do with health. Sarcopenia, or muscle atrophy, kills, whereas unhealthy insulin opposition may, but may not be associated with visible obesity and advanced blood sugar levels. It may happen in a slim-looking individual with average sugar levels, but it will not be diagnosed in time, as a simple and inexpensive measurement of the level of insulin in the blood, which should be done at the same time as the level of sugar, is not a standard test commissioned by doctors.
In the light of the above, it becomes clear that there are test results that make the optimal BMI value dependent on age [8, 9].
19 – 24 years: 19 – 24
25 – 34 years: 20 – 25
35 – 44 years: 21 – 26
45 – 54 years: 22 – 27
55 – 64 years: 23 – 28
over 64 years: 24 – 29
They can be justified as follows: the rate of metabolism decreases with age, so under the remaining unchanged conditions gradual fat deposition occurs. Maintaining muscle mass, the individual becomes more and more severe. It is worth noting the convergence of the value at the last item of the above calculation with the optimal value on the graph. Undoubtedly, a 70-year-old would have been healthier, more efficient, and had a chance for a longer life, having a BMI of 30, but only if he had kept his muscles at the same time, and this requires peculiar efforts and it is not always possible.
The definition of wellness by BMI tables would not be of large importance if it did not consequence in various, absurd attacks of weight loss, frequently in those who do not request it at all. Worse still, most recommended methods do not work in the long run, are counterproductive and unhealthy. The worst are all those ways that lead to the yo-yo effect, due to the fact that each weight failure is accompanied by a failure of muscle mass, which is then replaced by fat erstwhile re-weighting. However, a meaningful discussion of an highly broad subject of weight regulation and improvement of metabolic wellness requires a separate article.
Thanks for reading Jacek’s Substack! Subscribe for free to receive fresh posts and support my work.
[1] Body Mass Index = BMI = (mass in kilograms) divided by (height in meters) squared
[2] Obesity: Preventing and Managing the Global Epidemic. study of a WHO Consultation on Obesity. planet wellness Organization: Geneva, 2000,
http://apps.who.int/iris/bitstream/handle/10665/37003/WHO_TRS_854.pdf
[3] BMI and mortality: results from a national longitudinal survey of Canadian adults. Orpana HM, Berthelot JM, Kaplan MS, Feeny DH, McFarland B, Ross NA., Obesity (Silver Spring). 2010 Jan;18(1):14-8., Epub 2009 Jun 18. PMID: 19543208,
https://doi.org/10.1038/oby.2009.191
[4] The Morbidity and Mortality Associated With Overweight and Obesity in Adulthood. Matthias Lenz, Tanja Richter, Ingrid Mühlhauser, Dtsch Arztebl Int 2009; 106(40): 641–8, https://doi.org/10.3238/zartebl.2009.0641
[5] Excess Deaths Associated With Underweight, Overweight, and Obesity. Katherine M. Flegal, PhD; Barry I. Graubard, PhD; David F. Williamson, PhD; Mitchell H. Gail, MD, PhD, JAMA. 2005;293(15):1861-1867, https://doi.org/10.1001/jama.293.15.1861
[6] Cause-Specific Excess Deaths Associated With Underweight, Overweight, and Obesity. Katherine M Flegal 1, Barry I Graubard, David F Williamson, Mitchell H Gail. JAMA 2007 Nov 7;298(17):2028-37. https://doi.org/10.1001/jama.298.17.2028
[7] McCarthy, H., Ashwell, M. A survey of central fatness utilizing waist-to-height rates in UK children and adolescents over 2 decades supports the simple message – ‘keep your waist circumference to little than half your height’. Int J Obes30, 988–992 (2006). https://doi.org/10.1038/sj.ijo.0803226
[8] https://en.wikipedia.org/wiki/Wska%C5%BAnik_mass_cia%C5%82a
[9] Grimm and others, Food. Atlas and manual, 1st half, Wrocław: Elsevier Urban & Partner, 2012, ISBN 978-83-7609-653-7, OCLC 812586971